Bicuspid Aortic Valve
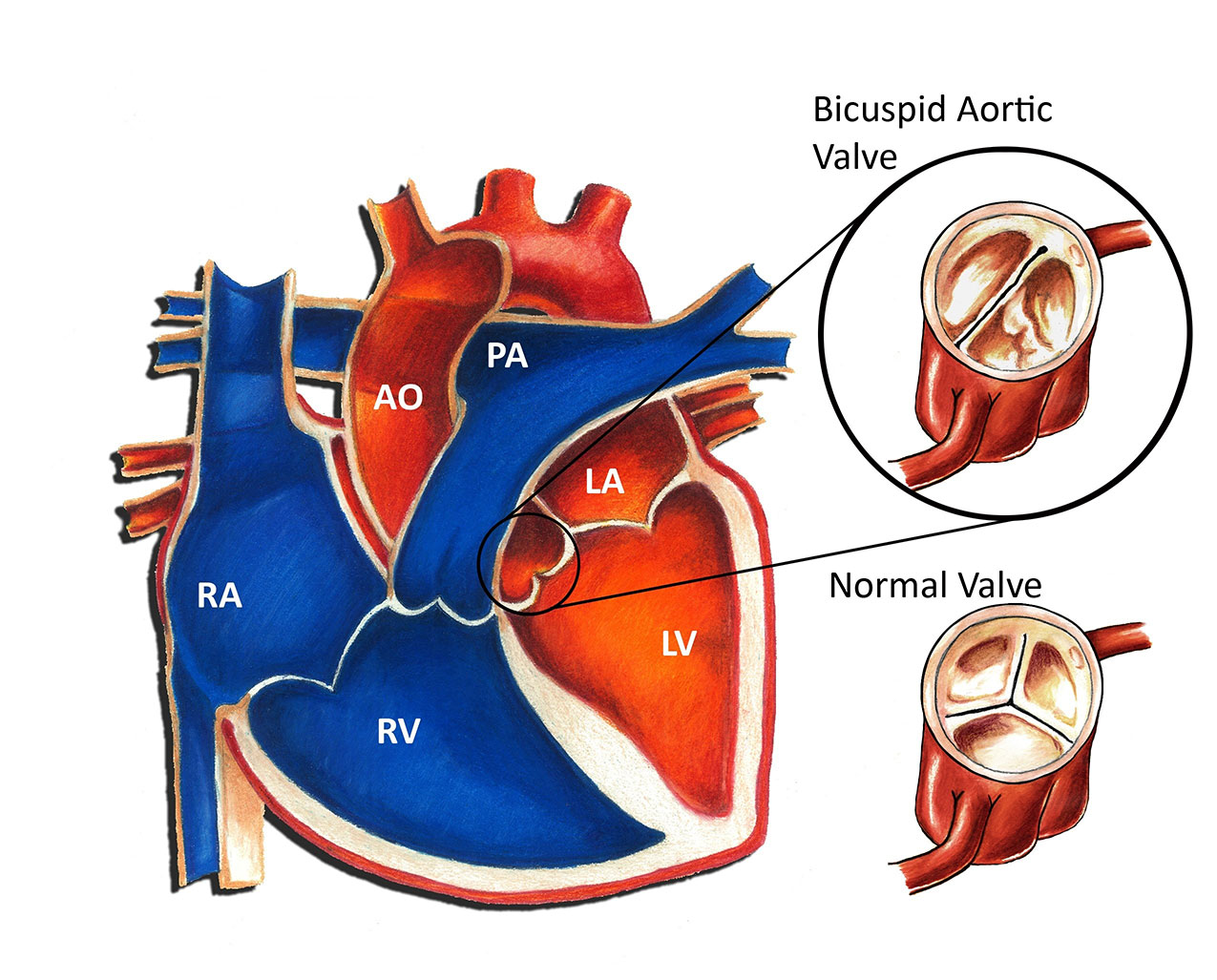
The aortic valve connects the left ventricle and the aorta. When the heart squeezes, the valve opens, allowing blood to pass from the left ventricle into the aorta. When the heart relaxes, the valve closes, preventing backflow of blood into the heart. A normal aortic valve has three separate leaflets. A bicuspid aortic valve has only two as opposed to the normal three leaflets. In many cases, two of the three leaflets are “stuck” together resulting in the bicuspid valve. A bicuspid aortic valve is a congenital heart defect, in other words, a birth defect of the heart. Congenital heart defects are the most common form of birth defects, occurring in approximately 1 in 150 individuals. A bicuspid aortic valve is one of the more common congenital heart defects. The exact incidence is not entirely clear, but some experts feel it may be the most common congenital heart defect overall. The cause of a bicuspid aortic valve is not known; some cases may be genetic in nature.
The significance of a bicuspid aortic valve is based on its functional status. Bicuspid valves have a tendency to develop either narrowing (“stenosis”) or leakiness (“regurgitation”). Physiologically, aortic valve stenosis creates a situation in which the left ventricle must squeeze more forcefully to pump blood past the narrowed valve. Aortic valve regurgitation creates a situation in which the left ventricle must pump a greater volume of blood with each heartbeat.
A bicuspid aortic valve in and of itself does not cause any symptoms. Symptoms are based on the functional status of the valve, in other words, the degree of aortic valve stenosis or regurgitation. The majority of patients with aortic valve stenosis or regurgitation rarely have any noticeable symptoms during infancy or childhood. Infants with severe aortic valve stenosis may develop a rapid respiratory rate or signs of impaired blood flow to the body. Occasionally older children with long standing, significant aortic valve stenosis or regurgitation may develop symptoms with exercise such as fatigue or even fainting.
Diagnosis of a bicuspid aortic valve can be made in a number of different ways. A patient with a bicuspid aortic valve usually comes to attention due to the presence of a heart murmur or an abnormal heart sound. There are many other different causes of heart murmurs, including normal causes. An echocardiogram uses sound waves to visualize the intracardiac structures and is the easiest way to diagnose a bicuspid aortic valve.
Most patients with bicuspid aortic valves gradually develop some degree of aortic stenosis or regurgitation over time. Usually this is a slow process that may even take decades to develop. A certain percentage of patients with bicuspid aortic valves never develop any functional abnormalities with the valve whatsoever.
Treatment options are based entirely on the functional status of the valve. Patients with a bicuspid aortic valve and mild stenosis or regurgitation require no specific therapy whatsoever. Patients that remain in this category have a normal life-span and are free to participate in most activities without restriction. Patients with severe or moderate to severe impairment of valve function require intervention to prevent long term damage to the heart. There are a number of different options, including both cardiac catheterization (valvuloplasty procedures) and surgery (valve replacement).
Up until recently, patients with any form of heart defect, including a bicuspid aortic valve, were recommended to use antibiotics prior to dental work or surgery to minimize the risk of heart-related infection. However, in May 2007 the American Heart Association changed this recommendation such that now most patients with congenital heart disease, including those with a bicuspid aortic valve, no longer require this precaution.
